After struggling for eight years to have a child, Shannon Petersen and her husband determined to strive in vitro fertilization (IVF) in 2022. Their fertility physician really useful a take a look at that seemed like precisely what they wanted. It promised to assist Petersen, then 42, keep away from miscarriages and get pregnant quicker by figuring out which of the couple’s embryos had been most certainly to lead to a wholesome child. The testing value 1000’s of {dollars} and wasn’t coated by insurance coverage, nevertheless it was marketed as near 100% correct and strongly really useful for girls of Petersen’s age. “I stated, ‘Yeah, that sounds wonderful,’” she says. “Who wouldn’t?”
Her temper modified when the outcomes got here again. The take a look at deemed every of the Petersens’ 5 embryos irregular, which means their clinic—like many within the business—refused to make use of any of them. “It was like, ‘Properly, higher luck subsequent time. These are rubbish, basically,’” Petersen says. “It was heartbreaking.”
The Petersens took out a $15,000 mortgage to strive once more. Their second IVF cycle yielded just one embryo, which they determined to not take a look at; it didn’t lead to a being pregnant. That disappointment felt like the tip of the highway. The couple started trying into fostering and adoption—till Petersen began researching the add-on take a look at she’d taken the primary time round: preimplantation genetic testing for aneuploidy (PGT-A). By some estimates, preimplantation testing is utilized in near half of IVF cycles within the U.S.
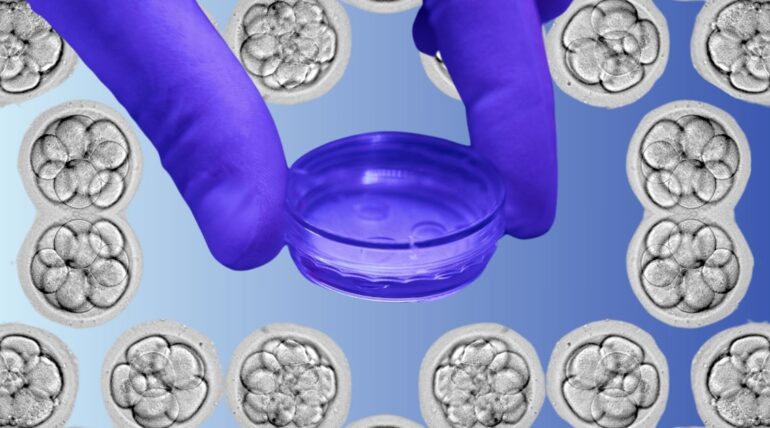
PGT-A is a screening take a look at carried out after a affected person’s eggs have been retrieved and fertilized to create embryos, however earlier than any of these embryos have been transferred to her uterus. Clinicians take tiny biopsies from the embryos, eradicating only a few cells to test whether or not they have the precise variety of chromosomes. Embryos with cells which have both too many or too few chromosomes are much less more likely to lead to full-term pregnancies, so PGT-A goals to determine them so clinicians can work with the strongest of the bunch.
However the extra Petersen learn, the extra she doubted the take a look at’s advantages. Quite a few researchers, she discovered, had questioned PGT-A’s accuracy, efficacy, and medical usefulness. In keeping with the American Society for Reproductive Drugs (ASRM) and the Society for Assisted Reproductive Know-how, the worth of the take a look at “has not been demonstrated” for routine screening of all IVF sufferers.
Petersen quickly discovered that scientists on the Stanford College Faculty of Drugs had been operating a medical trial to learn how typically so-called irregular embryos lead to wholesome infants. “No take a look at is ideal,” says Dr. Ruth Lathi, a professor of obstetrics and gynecology at Stanford and one of many lead investigators of that trial. “Our curiosity was actually pushed by affected person requests and affected person questions, and some remoted case stories of sufferers having profitable pregnancies [using] reportedly irregular embryos.” Analysis is ongoing, however Lathi hopes to trace 200 ladies with irregular embryos.
Learn Extra: Sufferers Are Suing Over Alleged Facet Results of Weight-Loss Medication
Newly disillusioned with PGT-A, the Petersens, who dwell in Northern California, enrolled in Lathi’s trial in 2024 as “a final ditch effort.” A health care provider affiliated with Stanford started transferring their outdated embryos. Their first try didn’t take. However, in a shock even to her docs, Petersen obtained pregnant on her second switch—utilizing an embryo that PGT-A had flagged as having a critical chromosomal abnormality.
She had a child boy in November. Her son has not gone by further genetic testing, however thus far appears wholesome and is hitting his developmental milestones. “I’d not have a child if I had believed the PGT-A take a look at,” Petersen says.
How may an embryo that was by no means presupposed to have a preventing probability grow to be somebody’s beloved son? That’s what the Petersens and practically 700 different IVF customers, together with loads of docs and scientists, wish to know. These sufferers have banded collectively to file class-action lawsuits in opposition to a number of U.S. suppliers of PGT-A testing—CooperSurgical, Natera, Reproductive Genetic Improvements (RGI), Ovation Fertility, Progenesis, and Igenomix—with legal professionals promising that fits in opposition to further testing corporations are coming quickly. Their authorized complaints argue that sufferers had been misled in regards to the accuracy and utility of PGT-A, dishonest them out of time, cash, and even desires of getting households, since some individuals have discarded embryos primarily based on the take a look at outcomes.
CooperSurgical, Natera, RGI, and Ovation Fertility have filed motions to dismiss the complaints in opposition to them, and Progenesis filed a movement for judgment on the pleadings, which seeks decision of a criticism earlier than trial. The entire instances had been continuing as of press time.
“PGT-A is a vital screening take a look at for IVF docs and sufferers,” a spokesperson for Natera stated in an announcement to TIME. “Medical doctors decide which sufferers will profit from PGT-A and, along with these sufferers, the way it must be used. We stand by the statements we’ve made about our take a look at, together with its accuracy, and the advantages PGT-A can carry to sufferers as proven in revealed, peer-reviewed research. The litigation in opposition to Natera is baseless.”
Representatives from RGI and Ovation declined to remark, citing ongoing litigation. CooperSurgical and Progenesis didn’t reply to a number of requests for remark. A consultant for Igenomix’s dad or mum firm referred TIME to a press launch, which says its authorized counsel is reviewing the case.
Allison Freeman, whose Florida-based agency Constable Legislation is spearheading the class-action fits, is an IVF mom herself. She turned “obsessed” with PGT-A after clinicians made her really feel “loopy” for opting out when she was a affected person, and solely extra so after two of her buddies ended up with no usable embryos after going by PGT-A testing. Curious, Freeman dug into on-line fertility communities, the place quite a few ladies reported upsetting experiences associated to PGT-A: cycles of failed assessments, inconsistent outcomes, and even unlikely births like Petersen’s.
Freeman was left with questions not solely about this explicit take a look at, but additionally about your complete IVF business. “It’s the Wild West of medication,” she says. “What if that is the tip of the iceberg?”
Within the U.S., oversight of the IVF business is dictated by a mix of state and federal insurance policies and “self-regulation” by skilled societies like ASRM (which didn’t make any of its spokespeople out there for interviews for this story). Underneath this patchwork system, adoption of a brand new know-how generally outpaces analysis and regulation round it, typically pushed by industrial pursuits, says Rosario Isasi, a lawyer and affiliate professor of human genetics on the College of Miami Miller Faculty of Drugs who researches the ethics of genomics.
PGT-A “began as an experimental process after which it moved to be thought of commonplace observe,” Isasi says. “Now, with the passage of time and extra research trying on the efficacy and security,” some specialists are debating whether or not that’s an excellent factor, particularly since there’s minimal regulation dictating how corporations develop, provide, and market these assessments.
Though labs that carry out PGT-A testing and medical gadgets utilized in IVF are topic to oversight by federal well being businesses, the U.S. Meals and Drug Administration has not approved any add-on preimplantation genetic assessments. States may craft their very own laws round IVF-related testing, however lawmakers have largely left the problem alone. One 2020 examine co-authored by Isasi, which in contrast preimplantation testing laws in 19 nations, concluded that the U.S. and Mexico have essentially the most hands-off insurance policies within the bunch.
Some see the proliferation of add-on companies as a money seize, since assessments like PGT-A are hardly ever coated by insurance coverage and may value 1000’s of {dollars} out of pocket. However proponents say they assist introduce some order to the chaos of human copy.
Similar to those that attempt to conceive the old school approach, {couples} who use IVF get no ensures. Regardless of the superior science behind the process—and the astronomical worth tags charged for it—IVF cycles typically fail. PGT-A was pitched as a approach to take away a number of the guesswork.
As an alternative of utilizing extra rudimentary strategies to evaluate embryo high quality—or transferring a number of without delay to extend the probabilities that at the least one would take—PGT-A guides clinicians towards embryos which are most certainly to lead to full-term, wholesome pregnancies. Medical doctors cross their fingers for “euploid” embryos (whose cells have the precise variety of chromosomes) and hope to keep away from “aneuploid” embryos (whose cells don’t). Between these black-and-white outcomes, there’s an entire world of grey: “mosaic” embryos which have a mixture of regular and irregular cells, “segmental” errors that have an effect on solely items of chromosomes, and extra. How a lot specificity a affected person receives relies upon, partially, on the clinic they go to and the lab that clinic makes use of, says Dr. Vasiliki Moragianni, medical director of the Johns Hopkins Fertility Middle.
In contrast to different prenatal assessments, PGT-A just isn’t explicitly meant to diagnose fetal well being issues, though it could possibly choose up on indicators of chromosomal problems akin to Down syndrome. At its core, it’s a rating device, says Darren Griffin, a professor of genetics on the College of Kent within the U.Ok., whose analysis contributed to the event of the know-how.
Think about a affected person who has 5 embryos after an IVF cycle. With out PGT-A, her physician could make educated guesses about which one is greatest. Perhaps they’ll get fortunate on the primary strive, or possibly it can take 5 separate transfers to seek out the one with the perfect shot of success—assuming, after all, she has the time, persistence, and cash to make it that far.
If she makes use of PGT-A, alternatively, her physician may determine the perfect embryo from the leap, ideally permitting her to keep away from the trouble and heartache of 4 failed transfers or miscarriages, Griffin says. On paper, the tip end result is similar—a dwell beginning—however the course of is way smoother because of PGT-A. That’s particularly helpful, Griffin says, for sufferers more likely to wrestle to conceive even with the help of IVF, akin to older ladies and people with earlier being pregnant losses. “In case you are in a better danger group,” he says, “it’s definitely value contemplating.”
Learn Extra: The Race to Clarify Why Extra Younger Adults Are Getting Most cancers
A lot of different docs vouch for PGT-A too, as evidenced by the truth that it’s so broadly used. And loads of research recommend that it could possibly fulfill its guarantees, specifically by serving to sufferers endure fewer embryo transfers and miscarriages on the trail to parenthood.
Dr. James Grifo, director of the NYU Langone Fertility Middle and a pioneer of genetic testing in fertility care, says PGT-A is widespread in his observe—about 90% of sufferers decide in after receiving details about the take a look at—and has significantly improved outcomes. “Yesterday, I did 11 being pregnant scans,” and all had been wholesome, he says. Again within the Nineteen Nineties, earlier than fashionable practices like widespread PGT-A testing, “if I had 11 pregnancies, I’d be telling 4 sufferers, ‘I’m so sorry, your being pregnant has an issue.’”
PGT-A’s advantages are “so apparent,” he says. “It’s onerous to consider it’s no more apparent to most.”
And but, the refrain of PGT-A skeptics is getting louder. Inside that group, there’s arguably nobody so vocal as Dr. Norbert Gleicher, an infertility specialist and medical director of the Middle for Human Copy in New York Metropolis. Gleicher has asserted that IVF beginning charges have fallen as add-ons like PGT-A grow to be extra widespread—in different phrases, he claims that the take a look at is making IVF worse reasonably than higher. “PGT-A is definitely dangerous to plenty of sufferers,” Gleicher says. “It’s sort of shameful. There usually are not many issues in drugs which are getting worse, and on the identical time getting dearer.”
Gleicher’s argument boils all the way down to this: PGT-A too typically manufacturers embryos irregular, and thus unusable, once they really aren’t. That raises a horrible prospect: are individuals needlessly throwing away embryos that would grow to be their youngsters?
Greater than a decade in the past, emboldened by research questioning the efficacy of PGT-A, Gleicher started transferring irregular embryos to consenting sufferers who had no euploid embryos left to work with. Usually, these experiments by no means resulted in being pregnant or led to loss. However generally, as he has since reported in a number of research, “we began seeing wholesome, chromosomally regular pregnancies.”
Researchers like Lathi, from Stanford, are doing extra analysis to find out whether or not such outcomes are “one in 1,000,000, one in a thousand, one in 100, or one in 10,” she says. However how may they occur in any respect?
Gleicher believes that even embryos PGT-A calls aneuploid generally have reproductive potential. In his view, biopsies of only a few cells—that are taken from the a part of an embryo that goes on to grow to be the placenta, not the fetus itself—are “completely inadequate” to make probably life-altering choices. (Some researchers even concern biopsies themselves might injury an embryo; the ASRM says there “are few knowledge on embryo biopsy strategies utilized in PGT-A.”) And he’s not alone in that view. “Is testing cells from the skin layer of the embryo consultant of the chromosomal make-up of the embryo correct?” asks Moragianni. “It’s attainable that it’s not.”
Though few go so far as Gleicher, specialists broadly acknowledge that embryo high quality is extra of a spectrum than a binary. “Each embryo has irregular cells in it,” Grifo says. So long as they’re uncommon, they’re doubtless inconsequential. If at the least 80% of biopsied cells are regular, most testing platforms will return a “euploid” end result.
Even larger ranges of abnormality don’t at all times make for critical issues. Research recommend that mosaicism is frequent in embryos, and that even these with a number of chromosomal abnormalities may end up in wholesome, full-term pregnancies—albeit much less typically than euploid embryos. In these fortunate instances, pure organic processes appear to permit the conventional cells to overhaul the irregular ones. “If the conventional cells take over, you get a child,” Grifo says. “If the irregular cells take over, it doesn’t make a being pregnant, normally, or it makes for a better probability of a miscarriage.” Gleicher’s analysis additionally suggests irregular cells generally self-correct within the womb.
Learn Extra: How you can Negotiate Your Medical Payments
Grifo says his clinic by no means discards embryos that match into this grey space and employs genetic counselors skilled to tell sufferers about their dangers and advantages. Most frequently, he says, sufferers decide to not use embryos with decrease odds of success.
So long as sufferers get sufficient correct info to enter testing with eyes open, Isasi says, there’s no drawback with clinicians providing it. The cornerstone of medical ethics “is knowledgeable consent—the flexibility of the affected person to weigh the dangers and potential advantages,” she says.
However not all clinics give sufferers a lot company. After two IVF cycles and $30,000 spent, Alexandra Zuk, a 39-year-old in South Carolina, and her husband had been “devastated” to haven’t any embryos their clinic thought of adequate to switch. They had been keen to take their possibilities with these they’d, Zuk says, however weren’t allowed. They considered switching to a extra versatile clinic however by no means discovered one to work with. “We don’t even know that I can carry a being pregnant as a result of I by no means had the choice to even strive,” she says.
Ultimately, reasonably than pay storage charges for embryos they had been informed they couldn’t use, the couple discarded them final yr. “We felt like we hit a lifeless finish,” she says. Now, Zuk, who’s certainly one of Freeman’s shoppers, is haunted by what-ifs. Had been these embryos actually nonviable? Wasn’t it value a strive?
Most researchers consider that if embryos are aneuploid, they won’t lead to wholesome infants. In a 2020 examine, Dr. Richard Scott, a former fertility physician who’s now scientific director on the Basis for Embryonic Competence, a New Jersey-based nonprofit analysis middle that additionally presents preimplantation testing, took biopsies from 484 embryos, however didn’t carry out PGT-A on them till after they’d been transferred. This allowed his group to trace what occurred to the embryos, then test whether or not any of the PGT-A outcomes diverged from actuality. They discovered that not a single aneuploid embryo resulted in a dwell beginning.
Such findings recommend PGT-A is “very, very highly effective” when carried out properly, Scott says. The issue, in his view, is that it isn’t at all times carried out properly. Most labs usually are not doing such rigorous research, and most corporations use industrial assessments that aren’t as well-validated because the one utilized in his analysis, Scott says. Whereas most PGT-A testing makes use of the identical core applied sciences, there’s variation in precisely how completely different testing platforms amplify and assess the DNA taken from the biopsied cells. If a validated PGT-A take a look at utilized in scientific analysis is a sports activities automotive, Scott says, many commercially out there platforms are like minivans: “All of them have 4 wheels, a steering wheel, and an engine. However they’re completely different in nearly each approach.”
Nonetheless, Scott says most client assessments do an excellent job of labeling regular embryos. There’s a small margin of error, as with nearly any take a look at—however within the overwhelming majority of instances, he says, an embryo branded as regular actually is. Scott believes the assessments’ actual “Achilles heel” is their false-positive charge: how typically they model embryos irregular once they really aren’t.
That prospect is regarding, as a result of PGT-A is unusually influential for a screening take a look at. If a most cancers display comes again with troubling outcomes, docs verify them with different assessments earlier than a affected person goes by intensive remedy. However PGT-A often is the closing phrase on the destiny of an embryo, since many clinics refuse to switch irregular ones—maybe for the sake of their success charges and legal responsibility protections, or maybe to defend sufferers from the emotional and monetary prices of failed transfers. After a spherical of PGT-A testing, a affected person might not have a single embryo their clinic is keen to switch. They might strive once more, if they’ve sufficient time, cash, and motivation. However in addition they might not.
Learn Extra: Dismissed and Disbelieved, Some Lengthy COVID Sufferers Are Pushed Into Psychiatric Wards
That’s a devastating resolution even assuming the testing is ideal. However some analysis helps Scott’s fears that it isn’t. In one 2022 examine, a group of researchers in China retroactively analyzed genetic materials taken from embryos that went on to lead to dwell births. In keeping with their testing, 11 out of 76 had been aneuploid. The truth that these “irregular” embryos resulted in infants, Scott says, suggests a major proportion of embryos are being misdiagnosed.
A number of analysis groups, together with Grifo’s, have additionally re-tested embryos beforehand analyzed by PGT-A and at the least sometimes discovered completely different outcomes the second time round. Grifo says such discrepancies are uncommon—in his group’s examine, 95% of embryos initially categorized as aneuploid nonetheless had been after repeated evaluation—and usually are not purpose to doubt the take a look at. However different analysis suggests these inconsistencies matter. In a single small 2024 examine of twenty-two embryos beforehand thought of “chaotic” (which means they’d six or extra abnormalities), the researchers discovered a 14% euploid charge throughout re-testing. At many clinics, sufferers could be strongly discouraged, and even forbidden, from utilizing chaotic embryos. However within the examine, two that re-tested as regular resulted in dwell births.
Disparate outcomes may level to various accuracy amongst testing strategies, Moragianni says. Or, if completely different biopsies from the identical embryo are examined every time, the included cells could possibly be completely different. “Each single cell of our physique [does not] comprise the very same info,” she says. “It’s attainable that we’re not precisely evaluating apples to apples.”
Jaime Magnetico-Walsh, who’s 42 and lives in Florida, has skilled that whiplash. In 2022, throughout their first IVF cycle, she and her husband had been thrilled to finish up with eight embryos, figuring at the least half could be wholesome. In actuality, just one handed the PGT-A take a look at. The couple transferred it, however Magnetico-Walsh’s being pregnant led to miscarriage. The couple donated their remaining seven embryos to science and began trying into egg donors.
Months later, after receiving complicated payments for embryo storage, Magnetico-Walsh was shocked to study that her fertility clinic had stored three of her mosaic embryos with out her information. “I used to be informed they have a tendency to maintain most of these embryos simply in case,” she says. “Till the couple has a dwell beginning, they preserve these as a result of, probably, they are often wholesome infants.”
This was stunning information for Magnetico-Walsh and her husband, who had beforehand been informed the embryos confirmed markers of Down syndrome and shouldn’t be transferred. Due to the back-and-forth, her clinic supplied to re-test them with PGT-A without spending a dime. This time, two of the three got here again as euploid—regular. “I used to be dumbfounded,” she says. She had donated her embryos to analysis, however “I felt like I used to be the science experiment.”
Magnetico-Walsh tried transferring a type of euploid embryos, however that being pregnant additionally led to loss. She has her remaining euploid embryo in storage, in addition to one from an egg donor, however feels paralyzed by the “emotionally, mentally, bodily, and financially taxing” rollercoaster she’s been on, which prompted her to hitch the lawsuits filed by Freeman.
Biology is complicated, and science evolves—particularly, Moragianni says, in a comparatively younger area like fertility care. Sufferers who use cutting-edge applied sciences like PGT-A need to grapple with each realities, confronting each the randomness of copy and the truth that analysis on add-on assessments like PGT-A is going on concurrently to the assessments being supplied. That overlapping timeline leaves unanswered questions.
5 years in the past, many clinicians would have suggested a affected person to discard mosaic embryos, says Dr. Rachel Weinerman, an infertility specialist and affiliate professor on the Case Western Reserve College Faculty of Drugs in Ohio. “Now, I feel the reply is, ‘Maintain onto them, as a result of there’s a probability that they could possibly be used,’” she says. “The query turns into, ‘What in regards to the ones that examined utterly irregular?’”
Proper now, she says, there’s little knowledge to help utilizing these supposedly nonviable embryos. However will that also be true in 5 or 10 or 20 years?
That’s a well-known query to sufferers like Katie Herrero, who’s 42 and lives in Pennsylvania. In 2019, she and her husband turned to IVF after a number of miscarriages, hoping assessments like PGT-A may defend them from further losses. They had been dismayed when two egg retrieval cycles collectively yielded just one chromosomally regular embryo, leaving Herrero and her husband with 10 that had been someplace on the spectrum of abnormality. They discarded these their docs stated had no probability at leading to wholesome pregnancies.
Later, nonetheless, Herrero discovered in an internet fertility group a few girl who had a child utilizing a reportedly aneuploid embryo that turned out to be a “complicated mosaic,” or one with a number of chromosomal abnormalities, however some regular cells. Herrero puzzled if any of the embryos she had discarded had been in the identical boat—and when she referred to as her lab for extra info, she discovered that one was. Her lab and clinic didn’t get that granular of their reporting again in 2019, so she was informed her embryo was aneuploid and, thus, unusable.
That have prompted her to contact Freeman in regards to the lawsuits in opposition to testing suppliers. Herrero hopes the litigation will assist enhance transparency within the business that she trusted to make her desires of motherhood come true—a dream that hasn’t but been fulfilled.
Right now, she says, she nonetheless thinks about what her embryos may have grow to be. “Had I identified what I do know now,” she says, “there could be no approach in hell I’d have discarded these embryos.”